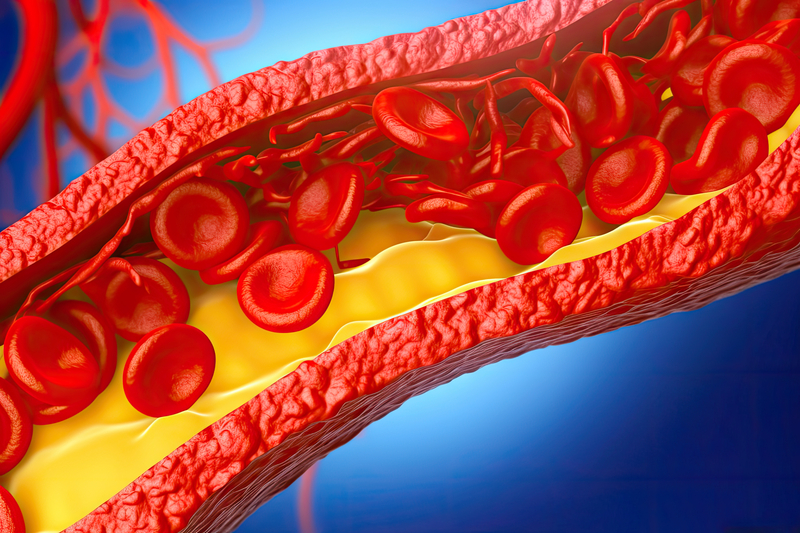
Heart Health
Disease Prevention
Lifestyle & Wellness
-
- The Best Multivitamins for African Americans
- The Unique Vitamin Needs of African Americans over 50
- Multivitamins May Help African Americans Avoid Alzheimer’s Dementia
- Displaced: Why African Americans Need Their Own Multivitamin.
- Vitamin D Deficiency is Associated with Stroke Risk in African Americans
- Low Vitamin D in African Americans