Topic: Cancer Prevention
Probiotics and African American Health
Probiotics and African American Health Probiotics can offer numerous health benefits for African Americans, including supporting gut health and enhancing digestion. They may help in reducing the prevalence of digestive issues that are more common in this population. Additionally, probiotics…

Garlic and African American Health
My African American patients are always talking about taking garlic rather than starting blood pressure or cholesterol-lowering medications. But what is the truth about the benefits of garlic? And how much should you take? It is true that garlic health…

Calcium Causes More Advanced Cancer in Black Men
Calcium and Prostate Cancer A number of studies have found that higher calcium intake was associated with an increased risk of advanced prostate cancer, specifically in Black men. Black men who consumed more milk and dairy products tended to have…

Benefits of Zinc for African Americans
Zinc and Infections In this age of deadly infections, it’s particularly important to have an adequate amount of zinc in your system because zinc possesses potent antiviral and antibacterial effects. African Americans have the highest risk for infections of almost…

Processed Meats: What They Are and Why They are Killing African Americans
What is a Processed Meat? In the health world, people are frequently told to decrease their consumption of “processed meats.” But what are processed meats? The most famous here in America is the simple hot dog. It's a combination of…

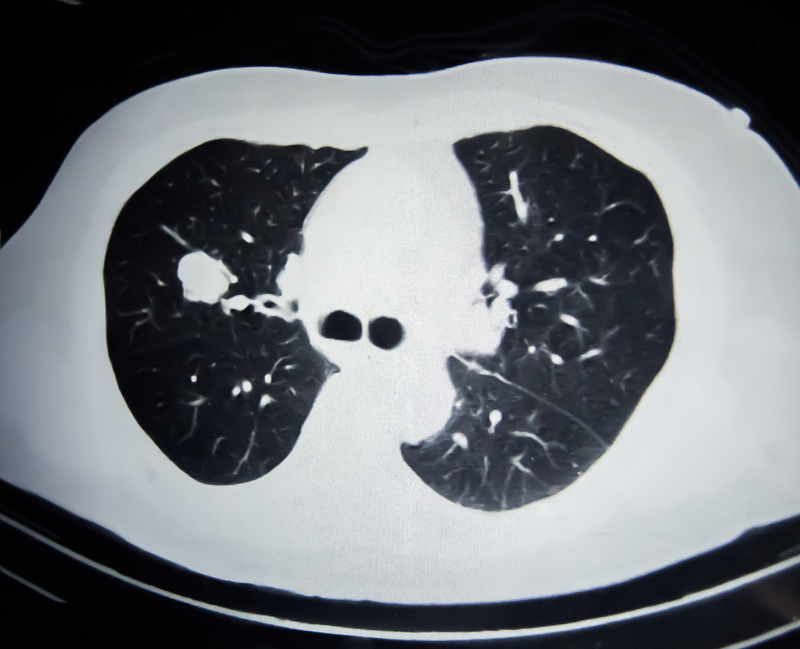
Lung Cancer & African Americans
Although the rate of lung cancer may appear similar between African Americans and White Americans at first, further analysis shows that African Americans actually have a 32% higher age-adjusted incidence of lung cancer. Additionally, African Americans are diagnosed with lung…

Preventing Breast Cancer in Black Women
Getting Breast Cancer Less, But Dying From it More Black women get breast cancer less often than White women yet they die from breast cancer at a much higher rate. How is that? They get breast cancer less, but die…

Colon Cancer in African Americans
Colon cancer has been called “the disease no one has to die from,” but African Americans continue to have the highest occurrence and the highest death rate compared to other racial/ethnic groups. Studies show that a Black man is 24 percent…

Continued Smoking After Cancer Raises Recurrence Risk
African American cancer survivors should make a deliberate effort to stop smoking because cancer recurrence or return was much higher in cancer patients who continued to smoke. In this study done at Wayne State in Detroit, Black patients were more…

Prostate Cancer in African American Men
Prostate cancer in African American men is more deadly, occurs more often, and can be easily detected by a blood test called a "prostate specific antigen" or "PSA." Yet many doctors have been advised against checking for this cancer because…