Colon cancer has been called “the disease no one has to die from,” but African Americans continue to have the highest occurrence and the highest death rate compared to other racial/ethnic groups. Studies show that a Black man is 24 percent more likely to get colon cancer than a white man and 47% more likely to die from it.

Colon cancer also occurs at a younger age in African Americans. The passing of Chadwick Boseman, the portrayer of the Marvel superhero Black Panther, at the age of 43 came as a surprise and shock to many, but not those in the health arena. We see young Black men and women getting diagnosed with colon cancer too often. And the stigma of having “cancer” keeps many quiet about their diagnosis.
Pele, who many say was the greatest soccer star, just passed from complications of colon cancer as well. His passing at 82, is still a great loss to his family and the world.
Reports have confirmed that Chadwick Boseman fought colon cancer for some years before his death but kept the diagnosis private for personal reasons. As a child, my grandmother had cancer yet survived into old age. As a young physician, I asked what type of cancer she had, and she looked at me with disbelief; how dare I ask such a personal question? For many in the Black community, even discussing cancer or its prevention is taboo.
Early Detection is Critical
If colon cancer is caught early, the prognosis is excellent, with over nine out of ten patients surviving five years. With many cancers, surviving five years is almost equivalent to a cure. But once it has spread to other organs and tissues, that survival rate plummets to only one out of four living five years.
African American men and women continue to be diagnosed at more advanced stages of colon cancer than other Americans. Even when adjustments are made for socioeconomic status, African Americans still have significantly lower screening.
Some of the reasons for low screening is an aversion to the methods we use to screen patients. I have had some patients look as if I insulted them by suggesting they get their stool sample tested.
“That part of my body is for OUT ONLY!”
In a study that included interviews with Black men ages 45-75 in Minnesota, Ohio, and Utah, researchers repeatedly heard concerns that colonoscopy, which involves the placement of a flexible tube inside the rectum, was associated with “gay sex” or was not masculine. “The stigma is because of the body part they’re examining,” researchers reported.
As an African American man who has had a colonoscopy, it is neither as invasive nor uncomfortable as the legend suggests. In fact, I have no memory of my colonoscopy thanks to anesthesia, and felt absolutely nothing but relief that my screening was successfully completed. I’ll die from something, but it won’t be colon cancer.
While I disagree with this dysfunctional and culturally-based viewpoint, I can also respect it as their unique perspective and find a way around it.
What about “Cologuard?”
With Cologuard, a person has a complete bowel movement into the container, seals it, and mails it in for testing. It only uses the “OUT” function of the rectum and shouldn’t offend anyone with those reservations. Researchers have looked at “multitarget stool DNA testing” (Cologuard is the trade name) performance in African Americans and found it to be “comparable to white patients.”
The Cologuard people then examine the genetic material (DNA) in the human stool and report the result back as “negative” (which of course is good in medicine . . . and don’t ask me why now), or “positive” and you will now need a full colonoscopy to find out if there is a true problem.

A colonoscopy is an outpatient procedure where a specialist looks at the entire length of the colon and rectum with a flexible scope, the width of a finger, with a light and camera at the end. They can see any pre-cancerous growths and remove them in real time. If your colonoscopy is normal, you won’t need another one for 10 years.
There are over 16 million colonoscopies done every year in the US with a very low complication rate. Colonoscopies would clearly be preferred over emergency bowel surgery which is the outcome if screening is avoided and cancer is present.
When should screening begin?
Your primary care provider should begin talking to you about colon cancer screening at age 45. If you have family members with a history of colon cancer, or an inflammatory bowel disorder like Crohn’s disease or ulcerative colitis, it should be even earlier than age 45. People who have had radiation to the stomach or pelvic area are also at risk for colon cancer.
Many people still wonder why cancer screening is needed? Many say: “I feel fine and I will call you once I have a problem.” The answer is simple, the earlier a cancer is found, the less of a problem it causes. Small cancers usually do not cause symptoms.
Some others feel that any cancer found means a death sentence . . . and that is not true. Early and small cancers of the lung, breast, colon, and others can simply be removed. With modern medicine, early cancers are much more easily treated. Large and late-detected cancers are more likely to give you symptoms, have spread to other organs, and more often result in death.
What About My Diet?
Immigration studies strongly support a major role for environmental factors (urban living, diet, etc.) as the root cause of increased colon cancer in the United States. People migrating from regions with a low prevalence of colon cancer, like Africa, to countries with a high prevalence, like the US, acquire the higher colon cancer prevalence of their new country within twenty years or less.
African Americans have 13 times the risk of colon cancer compared to native Africans.
Our high red meat consumption (beef, pork, and lamb) coupled with an elevated animal fat diet (chicken skin, hot dogs, lunch meat, butter, gravies, sauces) drives up the risk. That combined with decreased fiber consumption makes up the majority of the difference.
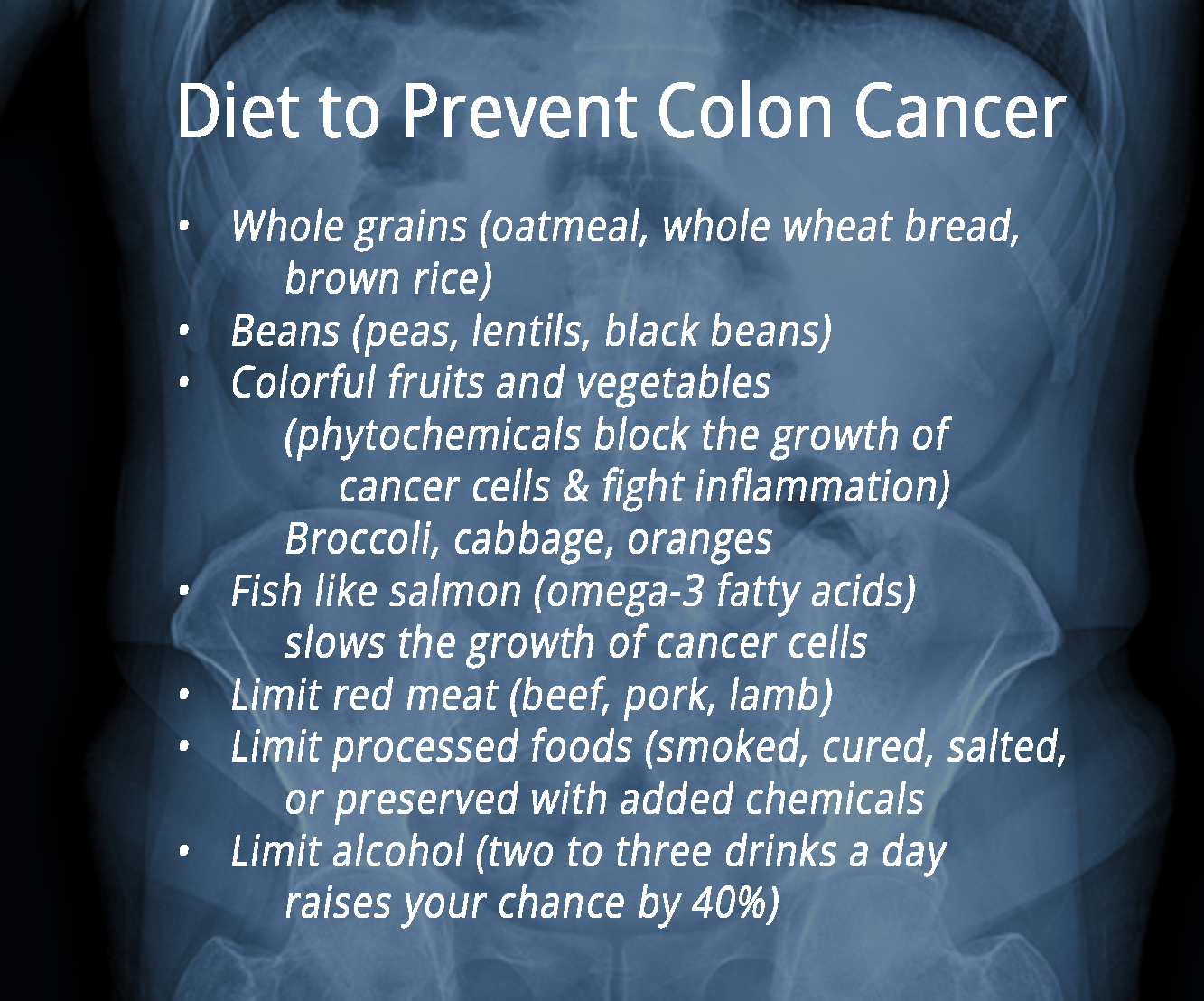
Vitamin D has numerous health effects, including strengthening bone, fighting infections, lower diabetes risk, and better blood pressure control, but African Americans have much more vitamin D deficiencies. Higher levels of vitamin D are also associated with a lower risk of colon cancer.
We Need to Get Over It!
Culturally, some African Americans have a defeatist attitude regarding good health. “I’ve struggled so much in my life; if I die, I die.” But this attitude unnecessarily leads to more struggle, suffering, and premature death. Breaking the cycle of seeing more African Americans die unnecessarily due to dysfunctional thinking is ALL of our responsibility. We cannot sit back and continue to watch while other communities take full advantage of what modern medicine affords.
 Yes, the Tuskegee study happened. Yes, bias and poor communication still exist in physicians today. But we as African Americans need to rise and move past these injustices. We shouldn’t avoid modern medicine; we should embrace it. If someone experiments on us, we can sue them. If a doctor acts dismissive toward us, find another doctor. It’s that simple. “Don’t throw the baby out with the bath water.”
Yes, the Tuskegee study happened. Yes, bias and poor communication still exist in physicians today. But we as African Americans need to rise and move past these injustices. We shouldn’t avoid modern medicine; we should embrace it. If someone experiments on us, we can sue them. If a doctor acts dismissive toward us, find another doctor. It’s that simple. “Don’t throw the baby out with the bath water.”
Ignoring medical advances only preserves the health disparities we so dislike.
Cancer Screening is Key
Get screened for colon cancer, breast cancer, lung cancer, and prostate cancer as suggested by your primary care provider. Let’s leave our dysfunctional biases behind.