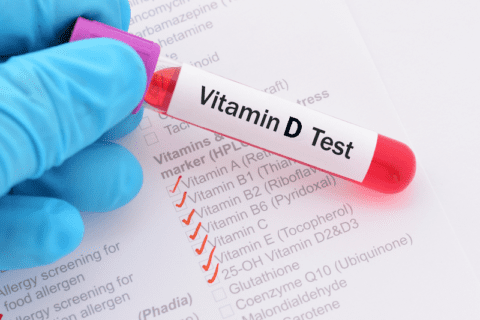
If you have diabetes, there is no question your doctor has measured your hemeglobin-a-1-c (HbA1c). The HbA1c measures the average blood sugar level over the past three months. It provides valuable information about long-term blood sugar control and helps healthcare providers assess diabetes control and a person’s risk of developing complications from the disease. By measuring the percentage of hemoglobin that is coated with sugar, the HbA1c test gives an overall picture of how well a person’s diabetes is managed.
WHAT IS A NORMAL HBA1C?
The target range for HbA1c levels varies depending on individual circumstances, but generally, a level below 7% is considered optimal for people with diabetes. Maintaining HbA1c within this range can significantly reduce the risk of complications such as cardiovascular disease, kidney damage, and nerve damage. Regular monitoring of HbA1c levels allows healthcare providers to make necessary adjustments to diabetes treatment plans and help individuals achieve better long-term blood sugar control.
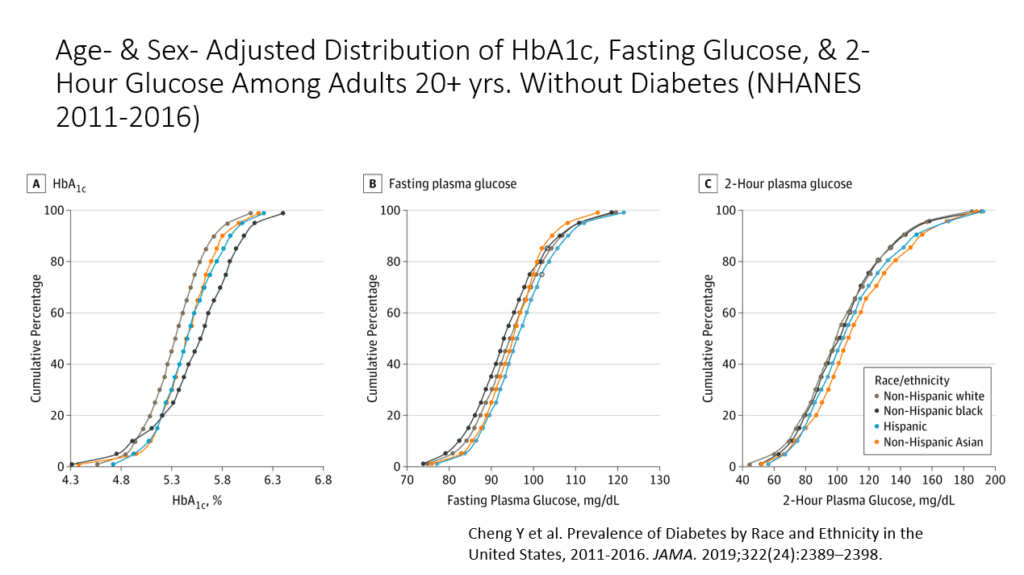
AFRICAN AMERICANS HAVE A HIGHER HBA1C
What isn’t well known is that African Americans tend to have higher HbA1c’s than other racial groups such that in reality, most African Americans should subtract approximately 0.4 from their laboratory-reported test result.
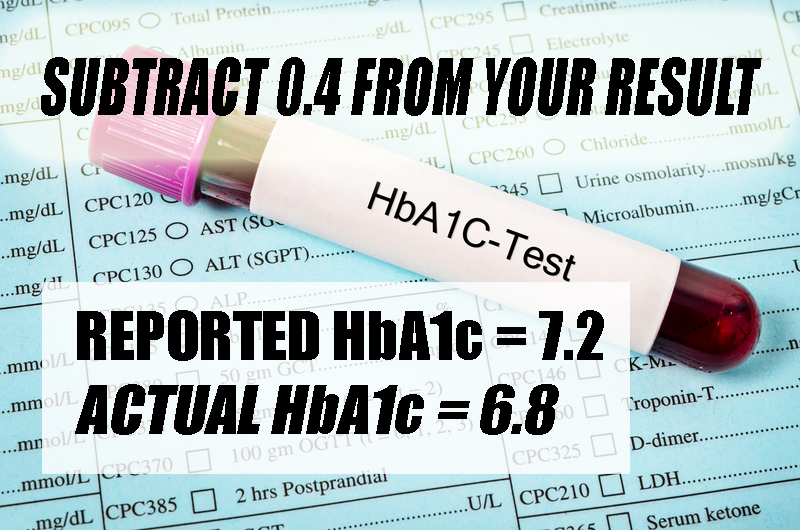
If your HbA1c is 8, you would subtract 0.4 and your actual result is closer to 7.6. If you levels are higher than 7.3, you probably need to get that result down lower, but once it gets into the 6s, you risk for hypoglcemia (having your sugar go too low) becomes more of a problem. As a group, African Americans have the highest risk for hypoglycemia, and hospitalization and possible death from low blood sugar.
There is growing evidence that suggests the HbA1c diabetes test may not accurately reflect some people’s true blood sugar levels.
SICKLE CELL AND HBA1C
People with sickle cell trait should be skeptical of HbA1c levels drawn on them. Their genetically modified red blood cells can affect the accuracy of HbA1c measurements. In individuals with sickle cell trait or sickle cell “disease,” the presence of abnormal hemoglobin can lead to falsely elevated HbA1c levels. This can result in an overestimation of blood sugar control and potentially lead to incorrect treatment decisions for diabetes management. It is important for healthcare providers to be aware of this relationship and consider alternative methods for assessing blood sugar control in individuals with sickle cell.
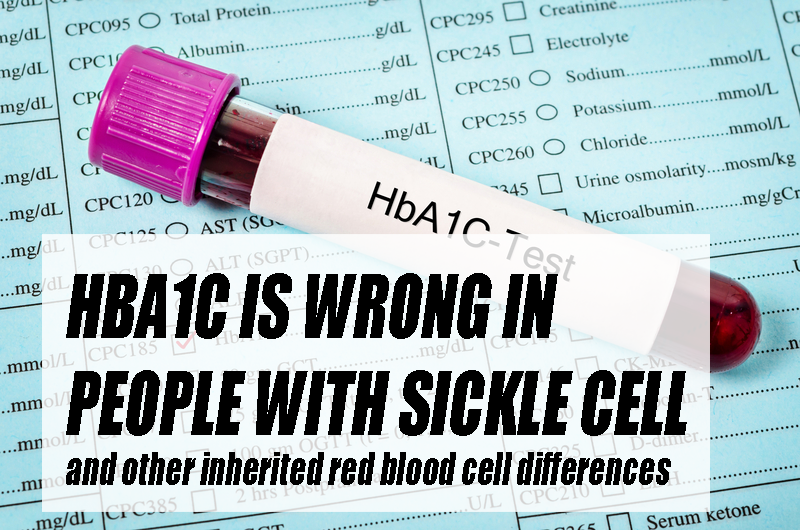
Sickle cell prevalence in African Americans is relatively high, with about 1 in 365 African Americans being born with the more severe form and 1 in 13 with sickle cell trait. Understanding the impact of sickle cell on HbA1c levels is crucial for accurate diabetes management in this population.
THALASSEMIA AND HBA1C
African Americans also have a higher rate of thalassemia, another condition that affects the red blood cells. The hemoglobin variants present in individuals with thalassemia may interfere with the accuracy of HbA1c measurements, making them falsely lower than reported.
GET YOUR HBA1C CHECKED REGULARLY
Aside from people with red blood cell differences (sickle cell, thalassemia, etc.), regular monitoring of HbA1c levels is crucial for individuals with diabetes as it helps healthcare providers assess the effectiveness of their treatment plans and make necessary adjustments. You should also keep track of your HbA1c levels so that you can adjust your diet. exercise, and medication routine. See my other article HERE about diabetes in African Americans. By tracking changes in HbA1c over time, healthcare providers can identify trends and patterns in blood sugar control, allowing for personalized and targeted interventions to achieve better long-term blood sugar management and reduce the risk of complications.
It is important that you discuss this with your physician before taking any action on your own. They have your best interest at heart, but may not be aware of the data supporting these claims. Work TOGETHER with your doctor. Have your provider click on the chart below so they can review the research
https://diabetesjournals.org/care/article/39/8/1462/37078/Are-There-Clinical-Implications-of-Racial