Topic: Cultural Competence
Lactose Intolerance in African Americans
Three out of four African Americans are lactose intolerant. Lactose intolerance means that if you drink milk, eat yogurt, have cheese, or any other dairy-based product in large amounts, your digestive system will have difficulty digesting it. Most people report…

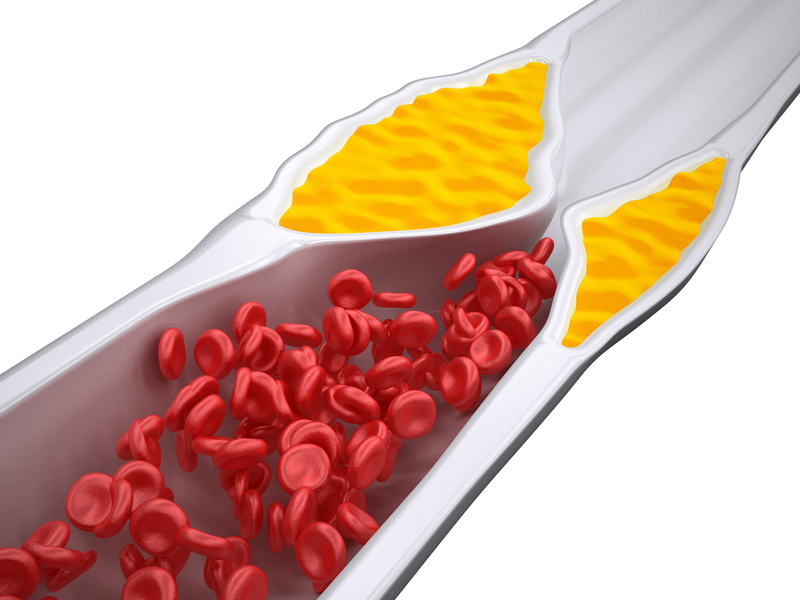
Is Cholesterol Lowering Medicine Bad for You?
Many of my patients have high cholesterol and are on cholesterol lowering medicines called statins like Lipitor (atorvastatin), Zocor (simvastatin), and Crestor (rosuvastatin). Occasionally they will come in saying some well-meaning friend told them that "cholesterol medicine is bad for…

Are you on the right blood pressure medicine?
High Blood Pressure in African Americans When it comes to the treatment of high blood pressure in African Americans, there are a number of important differences. For reasons that are not entirely clear, many African American patients respond differently from…

Strokes in African Americans
Strokes in African Americans Most strokes in African Americans occur due to high blood pressure and a much higher number of African Americans have uncontrolled blood pressure. A quarter of all strokes occur in the presence of atrial fibrillation (a fib)…

Heart Failure in African Americans
Heart failure in African-Americans occurs more often and is more deadly. African Americans have a significantly higher risk and earlier onset of heart failure and heart-related death compared to all other populations in the United States. In fact, African Americans are two…

Establishing Trust When Patients Distrust Doctors
Distrust Doctors ?? Multiple studies over an extended period of time confirm what most doctors and providers already knew, African Americans are more likely to distrust doctors and other healthcare providers than patients of other racial or ethnic groups. What…

Kidney Disease in African Americans
Kidney disease in African Americans is one the most dramatically different occurrences of a disease, and results in significant suffering and death. Generally, kidney disease is the result of diabetes and high blood pressure, and given the increased number of…

Atrial Fibrillation in African Americans
Atrial fibrillation in African Americans, also called "A Fib", effects one in nine before the age of 80 and is the most prevalent arrhythmia in the US and is associated with significant bad outcomes that include stroke, heart failure, and increased…

Prostate Cancer in African American Men
Prostate cancer in African American men is more deadly, occurs more often, and can be easily detected by a blood test called a "prostate specific antigen" or "PSA." Yet many doctors have been advised against checking for this cancer because…

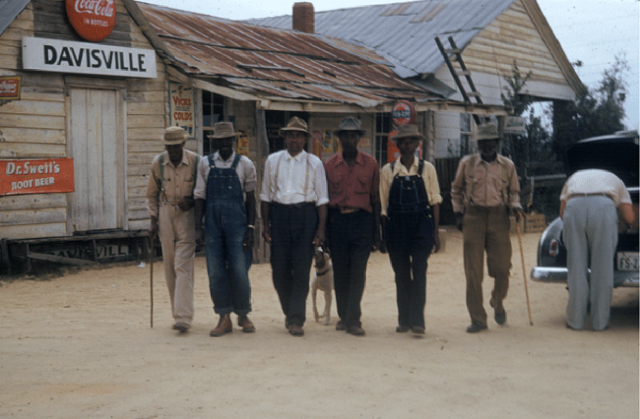
The Tuskegee Syphilis Study
The Tuskegee Syphilis Study (originally called "Tuskegee Study of Untreated Syphilis in the Negro Male") was originally formed to record the natural history of syphilis with the hope of justifying the funding of public treatment programs for African Americans. The…